
The largest cranial nerve in man, the trigeminal nerve has 3 major divisions: ophthalmic (CN Va/V1), maxillary (CN Vb/V2) and mandibular (CN Vc/V3). While CN V is primarily mediates tactile and nociceptive/thermal sensation of the face, CN Vc also has motor function in innervating the muscles of mastication.
Course
The trigeminal nerve leaves the brainstem as a large sensory root, and a small, medial motor root. The two roots pass forwards below the tentorium cerebelli and through an oval opening in the dura mater onto the apex of the petrous temporal bone, at the trigeminal impression.
The sensory cell bodies are located in the trigeminal ganglion, a mass on the sensory root. From its anterior edge branch the ophthalmic (Va), maxillary (Vb), and mandibular (Vc) nerves. The motor root joins the mandibular division.
The ophthalmic division passes through the cavernous sinus to exit through the superior orbital fissure. While the maxillary division passes forwards to the foramen rotundum, the motor and sensory mandibular division, exits the cranial cavity through the foramen ovale.
Standing Room Only (SOF, rotundum, ovale)
Mnemonic (skull base foramen for trigeminal nerve)
CLINICAL CORNER
Damage to the trigeminal roots can lead to anaesthesia in the face including the cornea, conjunctiva, mucosa of nose & mouth, and general sensation to the anterior 2/3 of the tongue. Function can be tested by touching the face with cotton wool on each side over forehead (corresponding to CN Va), medial cheek (CN Vb) and chin (CN Vc).
Trigeminal neuralgia is a neuropathic disorder characterised by episodes of severe facial pain, lasting from seconds and minutes to hours. There may be trigger areas on the face which may result in an episode when touched. Eating, talking or brushing the teeth may also trigger an attack. Anticonvulsant medication may alleviate pain.
Branches
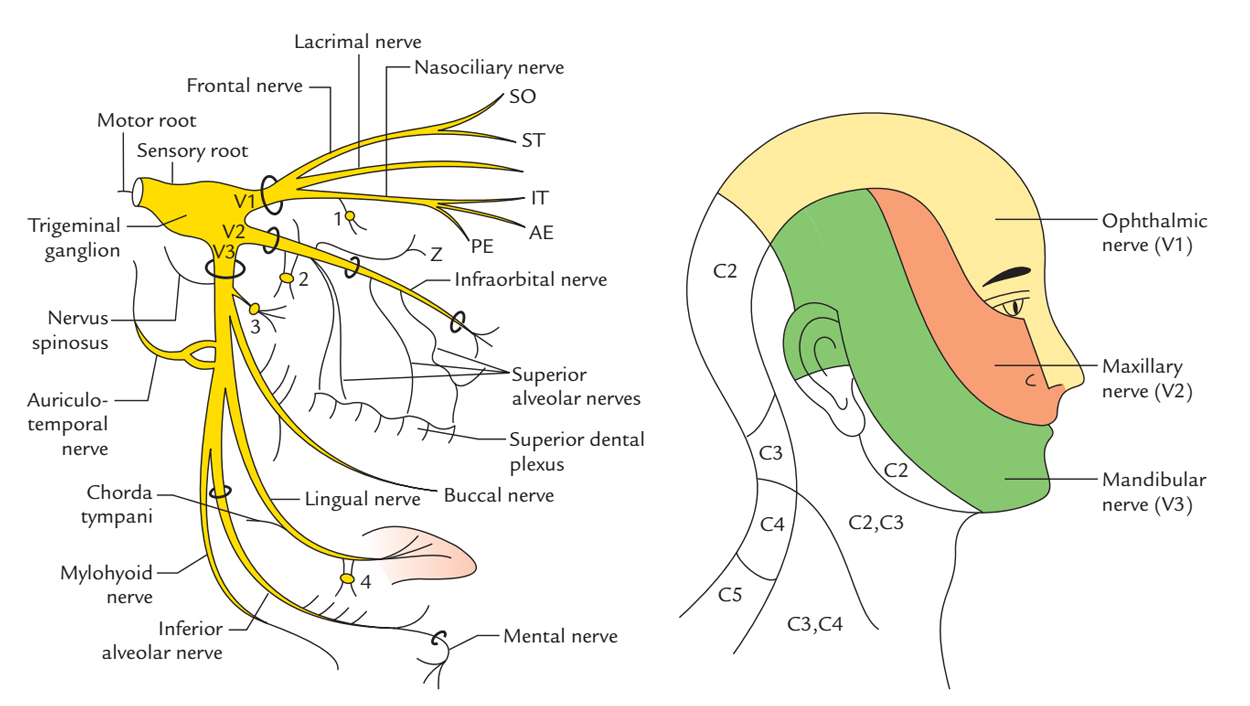
From ophthalmic nerve (CN Va)
- frontal: gives supraorbital (passes through supraorbital foramen) and supratrochlear nerves; supplies forehead skin and anterior scalp
- lacrimal: supplies skin of the upper eyelid and carries parasympathetic fibres from pterygopalatine ganglion to lacrimal gland
- nasocillary: supplies ethmoidal and sphenoidal sinuses; gives rise to long ciliary nerves carrying sensory fibres from the cornea and sympathetic fibres to dilator pupillae
CLINICAL CORNER
The corneal reflex is a defensive reflex that can be tested in awake/unconscious/semiconscious patients. A rapid, involuntary blink is generated in response to touching the cornea (e.g. with wisp of clean cotton wool or puff of air). It involves CN Va (nasociliary) afferent and CN VII efferent nerves on both sides.
From maxillary nerve (CN Vb)
- zygomatic: gives zygomaticotemporal and zygomaticofacial nerves; supplies the skin of the lateral part of the forehead and over the cheek
- ganglionic: gives branches to the pterygopalatine ganglion
- infraorbital: supplies maxillary teeth
From mandibular nerve (CN Vc)
Motor branches and the muscles they supply:
- nerve to medial pterygoid: medial pterygoid, tensor tympani, tensor palati
- deep temporal: temporalis
- lateral pterygoid: lateral pterygoid
- nerve to masseter: masseter
- nerve to mylohyoid: branches off lower alveolar before it enters the mandibular foramen, supplies mylohyoid & anterior belly of digastric
CLINICAL CORNER
Damage to the motor portion of CN V can follow strokes or tumours in middle cranial fossa. As the muscles of mastication is innervated, the jaw deviates to the weak side when mouth opens due to unopposed intact muscles. It is tested by palpitating the temporalis and masseter with clenched jaw or testing the power of jaw opening (lateral pterygoid muscles) against resistance.
Sensory branches and their areas of distribution:
- buccal: to mucous membrane and skin of the cheek
- auriculotemporal: to temporomandibular joint, skin of the upper half of the ear, external auditory meatus, scalp
- *inferior alveolar: enters mandibular foramen to supply lower teeth, branches mental nerve (through mental foramen in mandible) to skin of lower lip
- lingual (joined by chorda tympani from CN VII): general sensation to anterior two-thirds of tongue, floor of mouth, sensory branches to submandibular ganglion
CLINICAL CORNER
Since other nerve fibres hitchhike on trigeminal nerve branches, CN V lesions can also impact their function. In particular peripheral lesions of the lingual branch (CN Vc) may lead to loss of taste in anterior 2/3 of tongue and salivation that are mediated by chorda tympani.
