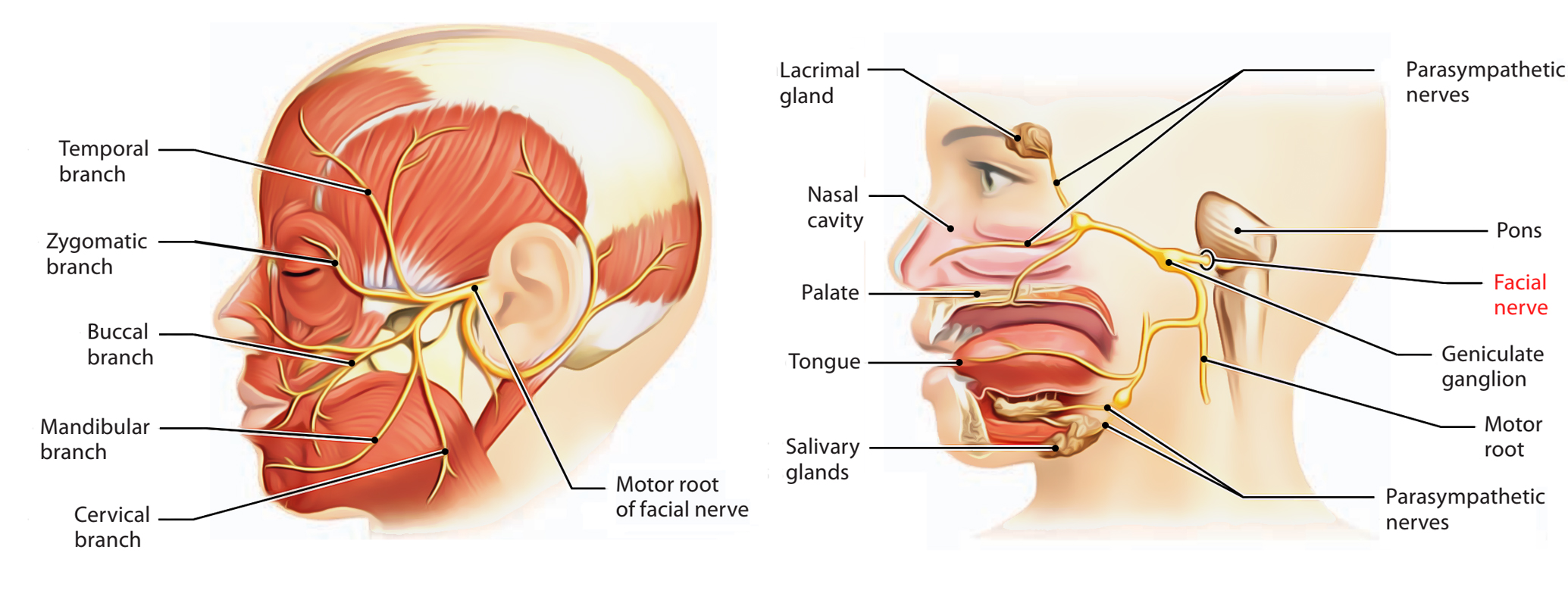
The facial nerve provides branchiomotor innervation to all the muscles (of facial expression) derived from the second pharyngeal arch. It also carries preganglionic parasympathetic fibres for the lacrimal, submandibular, sublingual and nasal mucous glands, and taste fibres from the anterior two-thirds of the tongue. Lastly, it is partially responsible for the general sensation of the skin lining the external auditory meatus.
Course

A larger motor root from the facial motor nucleus and a smaller nervus intermedius containing parasympathetic fibres (from the superior salivary nucleus) and sensory fibres (cell bodies in the geniculate ganglion) emerge from the brainstem to enter the internal acoustic meatus, before joining to form the facial nerve (travelling alongside CN VIII). Before emerging from the skull, the nerve travels along the narrow facial canal within the petrous temporal bone.
In the canal, the nerve travels to the medial wall of the middle ear and forms the geniculate (facial) ganglion, giving off the greater petrosal nerve, nerve to stapedius and chorda tympani. The remaining nerve fibres run posteriorly and on reaching the posterior wall of the tympanic cavity, inferiorly to emerge at the stylomastoid foramen.
Extracranially, the facial nerve first gives off the posterior auricular nerve (to the occipitalis) and branch to posterior belly of digastric and stylohyoid. It then enters the parotid gland and divides into upper (temporal, zygomatic and buccal branches) and lower (mandibular and cervical branches) divisions. The facial nerve is at risk of injury in parotid surgery, as its branches pass through the gland. It can also be injured in operations in the submandibular region, as its mandibular branch dips below the mandible before passing up to supply the lower lip muscles. As babies do not have a mastoid process at birth, the facial nerve is at risk of injury in forceps delivery.
CLINICAL CORNER
Damage proximal to the internal acoustic meatus (e.g. vestibular/acoustic neuroma on VIII, Ramsay Hunt syndrome: Herpes Zoster in facial nerve) can affect both CN VII & VIII nerves due to their closeness. Symptoms can include dry eyes due to parasympathetic denervation of the lacrimal gland via the greater petrosal nerve, facial paralysis and loss of hearing.
Branches
Intracranial branches
- greater petrosal nerve, arising at the geniculate ganglion and carrying parasympathetic fibres to the lacrimal gland via the pterygopalatine ganglion
- nerve to stapedius, a muscle which stabilises the stapes to dampen any over-vibration of the tympanic membrane and ossicles transmitting into the inner ear
- chorda tympani, which joins the lingual nerve. It mediates taste from the anterior two-thirds of the tongue and also carries preganglionic parasympathetic secretomotor fibres to the submandibular and sublingual glands.
CLINICAL CORNER
Middle ear damage may affect the chorda tympani or nerve to stapedius:
• Testing chorda tympani: Taste on the anterior 2/3 of the tongue can be tested using using liquids such as glucose, syrup or saline. Compromised secretion by the submandibular and sublingual glands may be observed.
• Testing nerve to stapedius: compare hearing on the 2 sides to check for hyperacusis.
Extracranial branches
- muscular branches to the posterior belly of digastric, stylohyoid and occipitalis.
- branches to the muscles of facial expression:
- temporal, to orbicularis oculi (closes eyelid) and frontalis (raise eyebrows)
- zygomatic, to the muscles of the eyelid
- buccal, to buccinators (prevents food moving to cheeks), orbicularis oris (puckers lips) and muscles of the external nose;
- mandibular, to the muscles of the lower lip and chin
- cervical, to platysma.
To Zanzibar by motor car
Mnemonic (facial nerve branches to facial expression muscles)
CLINICAL CORNER
UPPER vs LOWER MOTOR NEURON LESIONS
Bell’s palsy is an inflammatory disease of unknown cause, affecting the facial nerve in the facial canal. As a lower motor neuron lesion (i.e. not in the brain), it causes unilateral facial muscle paralysis.
After a stroke which is an upper motor neuron lesion (i.e. in brain) generally affecting one side, the upper part of the face can still be moved voluntarily (unlike in Bell’s Palsy), because those parts of the facial nucleus are bilaterally innervated by the forebrain.
Facial muscle paralysis can involve loss of facial expression, forehead wrinkles, a widened palpebral fissure (unopposed levator palpebrae superioris), overflow of tears, food accumulates in cheek (weak buccinator) and dribbling (weak lip closure). To test these, one can observe spontaneous movements of the face plus the patient can be asked to raise eyebrows, screw up eyes against resistance, smile, squeeze lips together and blow out cheeks. Since the facial nerve is also responsible for the motor component of corneal blink reflexes these can also disappear.
